High Phosphorus? Get the Facts
Phosphorus is a minerals found in food. It is also found in the human body. People with kidney disease often require a phosphorus restricted diet, Why? Because the kidneys can no longer eliminate the excess amounts consumed. Careful attention to phosphorus intake is important to prevent high phosphorus in the blood, also known as hyperphosphatemia.
Symptoms of High Phosphorus
Some of the symptoms a person with high phosphorus may experience include:
- Pain and stiffness in the joints
- Red eyes
- Itching
- Muscle weakness
- Bone fracture
- Spontaneous tendon rupture
Chronically high phosphorus levels in the blood can impact health and life expectancy. Risk of death increases at levels of phosphorus above 5.5 mg/dL. In addition, for every 1 mg/dL increase in phosphorus there is a 62% higher chance of death. High phosphorus can be particularly dangerous for the heart. A person with high phosphorus is 41% more likely to die from a heart-related cause when phosphorus levels are above 6.5 mg/dL.
Balancing Phosphorus
Phosphorus levels can be managed in several different ways. These include:
- careful attention to dietary intake
- dialysis for those people with stage 5 kidney disease
People who are in stage 5 kidney failure require dialysis treatments or kidney transplant. In the United States most people on dialysis attend in-center hemodialysis. This therapy includes 3 treatments each week for approximately 3 to 4 hours per treatment. Dialyzing 3 times per week will remove approximately 2,500 mg of phosphorus each week, or 833 mg per treatment. Longer, more frequent dialysis treatments (5-7 days a week) are provided during home hemodialysis (HHD). Another home therapy, peritoneal dialysis (PD), involves daily treatments. Both HHD and PD allow for more phosphorus removal from the blood, which may decrease phosphorus binding medication requirements.
Dietary Phosphorus
The average person can easily consume 10,000 mg or more of phosphorus per week (1,429 mg per day).
Average weekly phosphorus intake 10,000 mg
– Average removed in 3 dialysis sessions 2,500 mg
= 7,500 mg phosphorus balance in the blood
Dialysis is not able to remove the full amount of phosphorus in the blood, as can be seen in the above calculation. Therefore, a general guideline is to limit phosphorus intake to 800 to 1,200 mg per day (5,600 to 8,400 mg per week). The remaining phosphorus from the diet is often managed with medications referred to as “phosphate or phosphorus binders.”
Phosphorus Binders
Phosphorus binders are prescribed when blood levels exceed the normal range. Here are some important points about these binders.
- Binders are meant to be taken with meals, and sometimes with snacks. When taken with food or drink, phosphate binders act like a magnet to bind some (but not all) of the phosphorus in the food so that it is not absorbed. This happens in the gastrointestinal track during digestion.
- Commonly prescribed binders include: Calcium Acetate, Calcium Carbonate (Tums®), Renvela®, Renagel®, Fosrenol®, Auryxia®, Velphoro® and Phoslyra®.
- Most high protein foods have high amounts of phosphorus. Therefore it is especially important you take your binders with high protein meals or snacks.
Nutrition Facts about Phosphorus
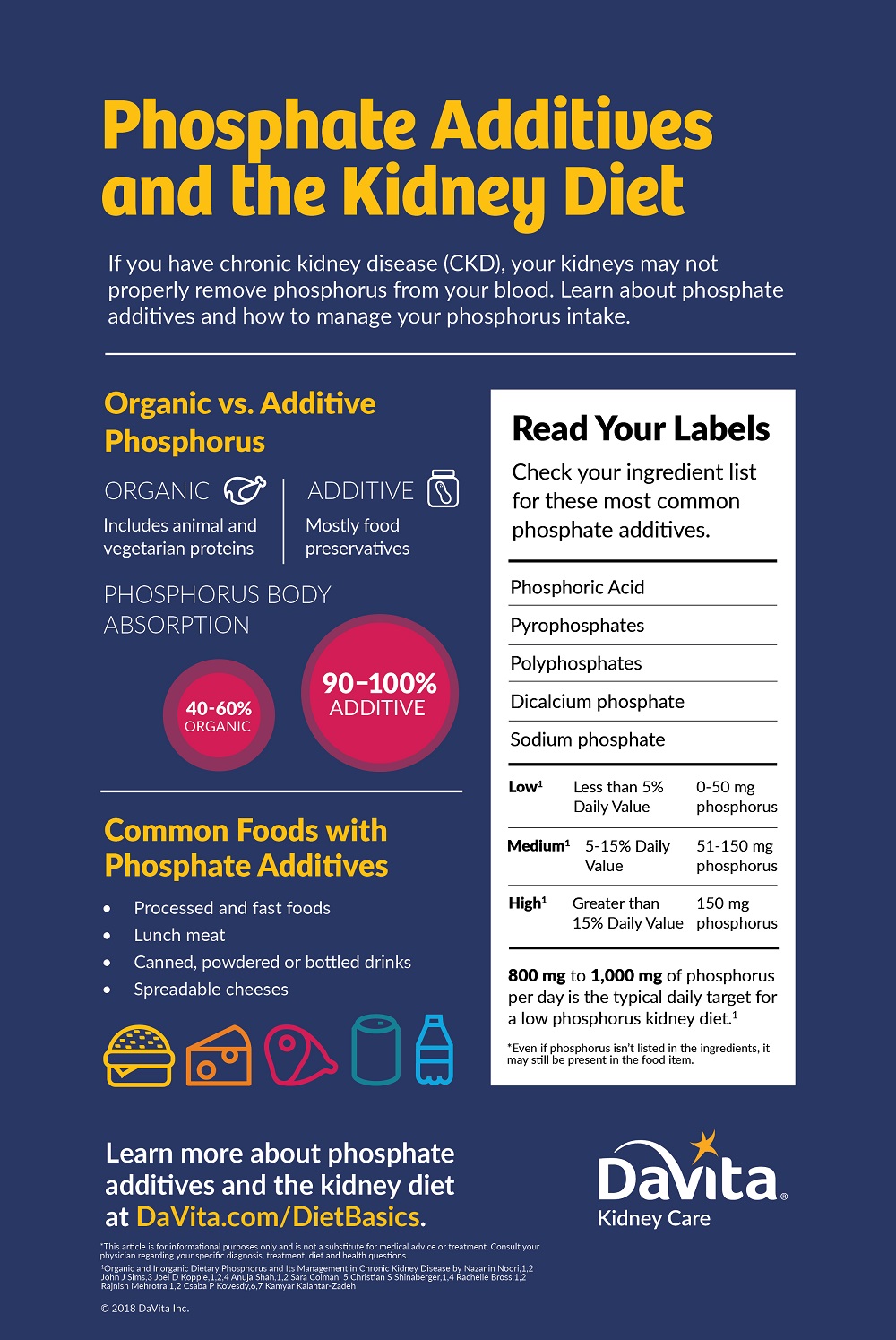
There are two types of phosphorus found in food and drinks: natural phosphorus (organic) and man-made phosphorus (inorganic).
Natural phosphorus is found in all foods, but in varying amounts. Foods that are naturally high in phosphorus include milk, nuts, seeds, beans, whole grains, chocolate, meat, poultry, fish and seafood.
Many companies add an artificial or inorganic form of phosphorus to food or drinks as a preservative, flavor enhancer, to improve texture, maintain juiciness and prevent separation of ingredients. Inorganic phosphorus is often added to deli meats, bacon, sausage, dark sodas such as cola, processed cheeses, chips, cookies, breads and baked goods, and many other pre-packaged foods. Fast food places and many restaurants also serve foods that contain inorganic phosphorus.
When a natural source of phosphorus is eaten, the body absorbs 40-60% of what’s consumed. When an artificial source of phosphorus is eaten, the body absorbs 90-100% of what’s eaten! Unfortunately food labels are not required to list phosphorus but some do include it. You can read the ingredient list if phosphorus content is not included on the nutrition facts label. Compare brands to find a product that does not contain artificial phosphorus, if possible.
Reference:
Byham-Gray, L., Stover, J., & Wiesen, K. (2013). A clinical guide to nutrition care in kidney disease. Chicago, IL: Academy of Nutrition and Dietetics.
Additional Kidney Diet Resources
Visit DaVita.com and explore these diet and nutrition resources:
DaVita Kidney-Friendly Recipes
This article is for informational purposes only and is not a substitute for medical advice or treatment. Consult your physician and dietitian regarding your specific diagnosis, treatment, diet and health questions.

Recent Comments