Achieving Improved Results with an ESRD Integrated Care Model
End stage renal disease (ESRD) patients present with a unique set of complexities that can be better managed through an ESRD-specific integrated care model. The support of an integrated care management infrastructure can help physicians and other clinicians in their efforts to achieve the following:
- Improved care efficiency for the whole patient
- Increased coordination and communication across the continuum of care
- Enhanced patient understanding and engagement
- Improved clinical outcomes and enhanced patient quality of life
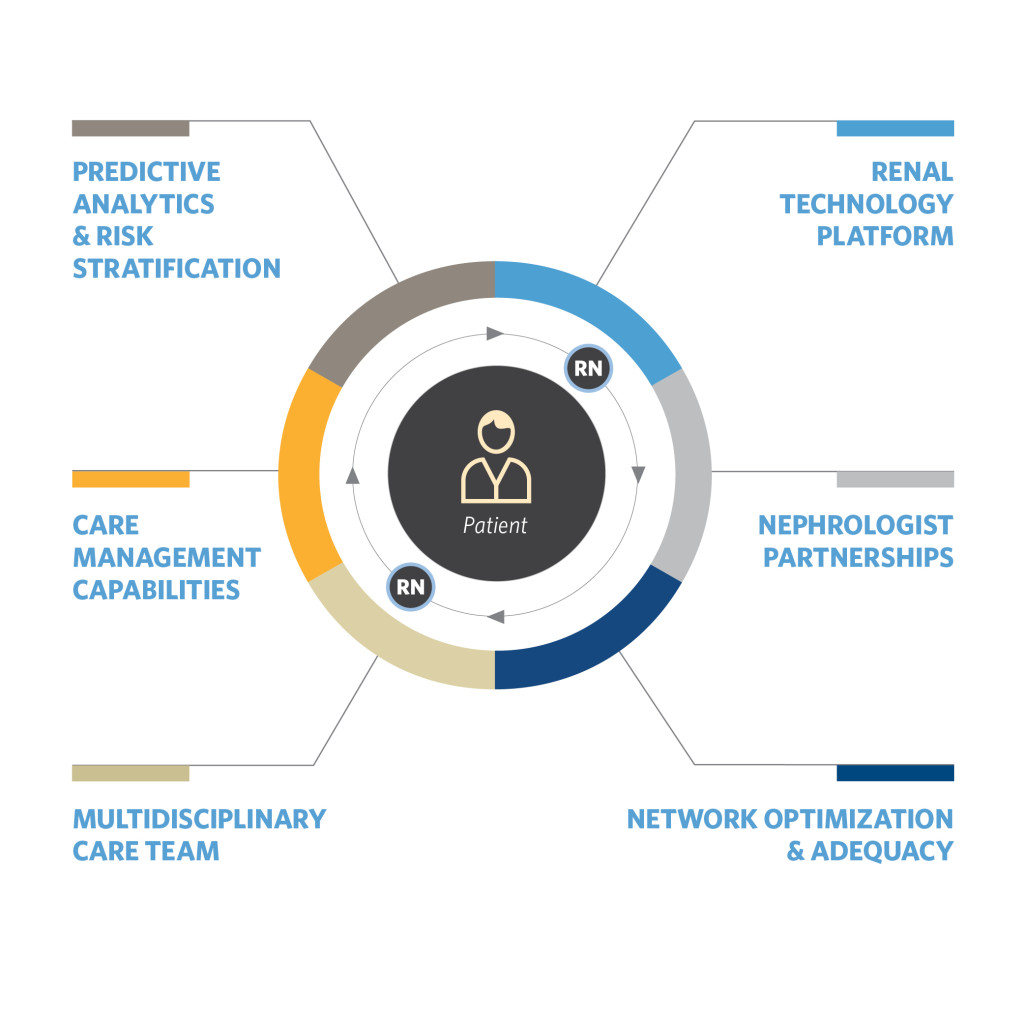
An optimal integrated care model is supported by the following capabilities.
Predictive Analytics and Risk Stratification Renal-specific risk stratification algorithms and predictive models identify patients for specific care management interventions. Custom models forecast CKD patients most likely to transition to dialysis and ESRD patients most likely to be hospitalized.
Renal-Specific Care Management Capabilities Renal nurse care managers, nurse practitioners and non-clinical care coordinators provide support for patients—ideally in dialysis centers where patients treat 12 to 15 hours each week. Call centers can provide added support. Nurses and care coordinators can use a renal technology platform to advance clinical protocols and patient care pathways, which are customized based on a patient’s state of health and care plan.
Multidisciplinary Care Team Renal nurse care managers coordinate care across dialysis center care teams (clinic nurses, patient care technicians, dietitians and social workers), nephrologists, specialists, behavioral health providers, hospitals and pharmacists to manage the medical and psychosocial needs of enrolled patients. While telephonic care management is invaluable, physically integrating the team into each dialysis center—when scale permits—further optimizes program results.
Renal Technology Platform A renal technology platform should integrate with CKD and ESRD-specific care pathways and clinical protocols, predictive analytics and risk stratification algorithms to enable renal nurse care managers and care coordinators to uniquely tailor care for each patient. The technology platform integrates with a mobile care team rounding tool and multiple clinical data sources and systems.
Nephrologist Partnerships Renal nurse care managers work with nephrologists to establish and manage each patient’s care plan and provide monthly integrated care reports.
Network Optimization and Adequacy ESRD patients must have access to quality nephrologists, specialists and dialysis centers. Dialysis centers should partner existing provider networks to make sure patients receive high-quality, timely and coordinated care. Patients should use publicly reported quality data, such as the Centers for Medicare & Medicaid’s Five-Star Quality Ratings, when selecting a dialysis center so they can choose a center that best meets their needs.
With increased accountability for outcomes in healthcare, physicians and other clinicians—more than ever—are focusing attention on improving outcomes for their patients. With support from a strong integrated care infrastructure, they can help enhance ESRD patient quality of life by current measures and can innovate to help achieve still greater quality in the future.

Recent Comments