Study: Use of Predictive Analytics to Inform Integrated Care Programs to Reduce Hospitalizations among Hemodialysis Patients
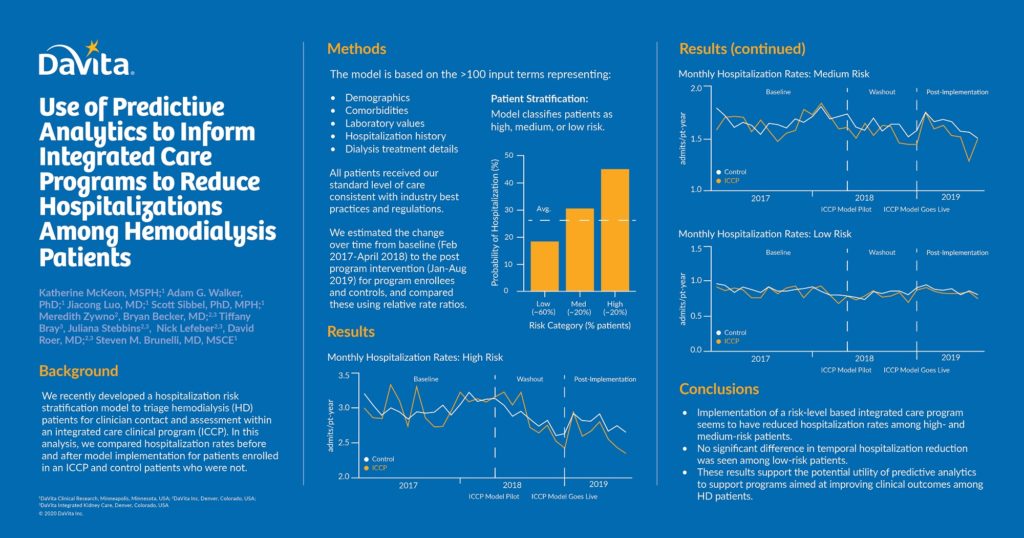
Integrated care for dialysis patients could benefit from identification of those who are at high risk for poor outcomes in order to efficiently deploy clinical resources. DaVita Clinical Research in collaboration with DaVita Integrated Kidney Care (IKC) and DaVita Inc. recently developed a hospitalization risk stratification model to triage hemodialysis (HD) patients for clinician contact and assessment within an integrated care clinical program (ICCP). In this analysis, hospitalization rates were compared before and after model implementation for patients enrolled in an ICCP and control patients who were not.
The risk stratification model is based on more than 100 input terms representing:
- Demographics
- Comorbidities
- Laboratory values
- Hospitalization history
- Dialysis treatment details
The model classifies patients as high, medium or low risk. With an area under the curve (AUC) of 0.81, the model has a very good overall performance and ability to discriminate.
All patients received our standard level of care consistent with industry best practices and regulations. ICCP patients predicted to be medium and high risk received additional services (e.g., telephonic health programs, case management, health screens, resource navigation) proportional to predicted risk level. Relative differences in annualized hospitalization rates for HD patients enrolled in an ICCP were compared to controls who were not by calculating relative rate ratios (RRR) and 95% confidence intervals (CI) in the baseline (Feb 2017-April 2018) and postmodel implementation (Jan-Aug 2019) eras. Comparisons were stratified by predicted risk level. Potential effects we anticipated, a priori, in the high-and medium-risk groups. The low-risk group was included as a negative control because low-risk status should not have led to differential clinical action based on program design.
The baseline hospitalization rate was 3.0 admissions/patient-year (pt-yr) for all high-risk patients. Post implementation, hospitalization rates decreased to a greater extent among ICCP patients (-0.4 admissions/pt-yr) versus controls (-0.2 admissions/pt-yr): RRR (95% CI) = 0.94 (0.90, 0.97). The baseline hospitalization rate was 1.7 admissions/pt-yr for all medium-risk patients. Post implementation, hospitalization rates decreased to a greater extent among ICCP patients (-0.2 admissions/pt-yr) versus controls (-0.1 admissions/pt-yr): RRR (95% CI) = 0.95 (0.90, 1.00). No differences were observed among low-risk ICCP patients and low-risk control patients.
These results support the potential utility of predictive analytics to support programs aimed at improving clinical outcomes among HD patients.
For more information, see the ePoster (which was presented at the American Society of Nephrology’s virtual meeting in 2020), here.

Recent Comments