This weekend my wife and I visited some friends in Santa Barbara who are supporters of The Music Academy of the West. The Academy was founded by a group of artists and patrons in 1947 to “…aid in the development of gifted young classical musicians through advanced study with accomplished faculty artists.…” The Academy has evolved and now has its own campus where each summer more than 130 fellows participate through a combination of personal instruction, educational programs and live performances before small or large audiences. Guest faculty includes some of the icons of the music world, such as vocalist Marilyn Horne, opera legend Kiri Te Kanawa, violinist Gil Shaham, pianist Ingrid Fliter, and percussionist Colin Currie. Underlying it all is a strong culture of mentoring, as there is in training for a professional music career even while in school.
Participating students are experiencing this incredible summer experience while on hiatus from New England Conservatory, Juilliard, The Cleveland Institute of Music, Manhattan School of Music, Eastman School of Music and many other prestigious institutions. As I read through each student biography, I was struck by the fact that not only was the person’s school listed, but the key teacher with whom each student worked was identified as well. Mentoring. I had a chance not only to listen to solo, ensemble and orchestra performances, but also to talk to some of the students about their dreams for the future. There was a sense of wonder, of anticipation, of passion about the career for which they were preparing that inspired me. But it also made me think about my own career and the future of nephrology.
This was not the first time I was introspective about the need to re-examine nephrology as a discipline; to rethink how we attract the best and the brightest to the specialty and create opportunities for young doctors to see why nephrology, and improving the lives of kidney patients, is a noble, desirable career. In 2004 my colleagues and I published the results of a survey we took of 67 fellows participating in an advanced perceptorship in nephrology.1 We found that exposure to hemodialysis and peritoneal dialysis was pathetic, with 50% of fellows reporting fewer than three months of exposure to in-center hemodialysis ICHD, often without didactic sessions or regular attending rounds) and 25% no exposure at all to peritoneal dialysis. This mirrored concerns expressed by many more than 10 years previously. 2-4
Well, here we are, another 8 years later and has the situation improved? Three recent articles address this issue. Merighi et al. attempted to study the relationship between nephrology training experience and subsequent clinical practice. 5 Using a national survey, data from 2010 provided insights into the experience of over 600 nephrologists. Nearly 40% of respondents answered they did not feel well prepared for the care of dialysis patients at the end of their fellowship. In addition, although over 90% of dialysis patients in the US utilize ICHD, only 6% of the nephrologists surveyed would choose this modality for themselves.
Is this just a problem with training programs or is it a problem with the expectations residents have as they consider nephrology as a career? Shah et al. have tried to address this question in a fascinating study published recently. 6 Over 50% of the time nephrology was chosen prior to the second year of medical residency training, in half of these individuals during medical school or before. While the majority chose nephrology because of the interesting subject material, only 65% reported that mentoring or a role model was influential in the decision. A disappointing 64% were extremely or very satisfied about their career choice; however, the most common reason for high levels of satisfaction was mentoring.
So, how can the torch of nephrology be brightened, enhancing interest in the specialty, attracting the best and the brightest who can drive innovation in outcomes for our patients? Jhaveri et al. have proposed an interesting elective experience for medical residents that is an important step in the right direction.7 While there are many creative components to this approach, enhanced mentoring is an important component.
The theme is inescapable: if we really want to attract the nephrologists we would like to care for our families and ourselves, we need to focus on role models and mentors who are passionate about nephrology, about service to patients and about innovating to improve outcomes. If we can instill these cultural values in young physicians early in their career decision-making process, we can perhaps begin to build the discipline of nephrology to new greatness.
As Robert Frost said,
“I am not a teacher, but an awakener.”
It is incumbent on all of use to awaken the passion in students and colleagues to build the discipline our patients deserve.
Plutarch, over 2000 years ago, said it best:
“The mind is not a vessel to be filled, but a fire to be kindled.”
Striving to bring quality to life,
Allen R. Nissenson, MD
Follow me on Twitter
To make sure you receive a notification when a new blog is posted, click here
To comment on this post click here
- Nissenson AR et al. Improving Outcomes in CKD and ESRD Patients: Carrying the Torch from Training to Practice. Semin in Dial 17:380, 2004.
- Fine LG. A Proposal to Improve the Attractiveness of Nephrology as a Subspecialty Choice for Residents in Internal Medicine. Am J Kidney Dis 15:302, 1990.
- Nissenson AR. Morbidity and Mortality of United States Dialysis Patients. The Legacy of Inadequate Nephrologist Training? Semin in Dial 5:277, 1992.
- Kimmel PL et al. Effectiveness of Renal Fellowship Training for Subsequent Clinical Practice. Am J Kidney Dis 18:249, 1991.
- Merighi JR et al. Insights into Nephrologist Training, Clinical Practice, and Dialysis Choice. Hemodial Internat 16:242, 2012.
- Shah HH et al. Career Choice Selection and Satisfaction among US Adult Nephrology Fellows. www.cjasn.org Vol 7 September, 2012.
- Jhaveri KD et al. Enhancing Interest in Nephrology Careers During Medical Residency, in press. http://dx.doi.org/10.1053/j.ajkd.2012.04.020.

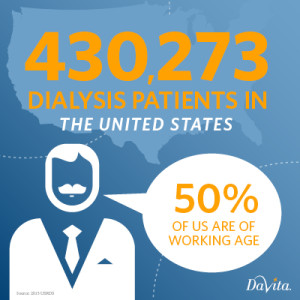 I was speaking to a group of end stage renal disease (ESRD) patients at a symposium recently and met a 50-year-old man with polycystic kidney disease who had just started on in-center hemodialysis. He had been followed by a nephrologist for a number of years prior to progressing to ESRD, and had been well prepared by conventional standards to start dialysis while being placed on the cadaver transplant list. He had an arteriovenous fistula, and began dialysis uneventfully as an outpatient. He said that physically he was adapting well to dialysis, but was concerned and depressed because he quit his job when he knew dialysis was imminent. His doctor had not had a conversation about this issue with him and he didn’t know what to do or how he was going to continue to take care of his family. He asked me why dialysis patients had to stop working and he was surprised to hear me say that he could continue working, and that his doctor and dialysis facility should be helping him work through this issue and get back to work. This story is only too common.
I was speaking to a group of end stage renal disease (ESRD) patients at a symposium recently and met a 50-year-old man with polycystic kidney disease who had just started on in-center hemodialysis. He had been followed by a nephrologist for a number of years prior to progressing to ESRD, and had been well prepared by conventional standards to start dialysis while being placed on the cadaver transplant list. He had an arteriovenous fistula, and began dialysis uneventfully as an outpatient. He said that physically he was adapting well to dialysis, but was concerned and depressed because he quit his job when he knew dialysis was imminent. His doctor had not had a conversation about this issue with him and he didn’t know what to do or how he was going to continue to take care of his family. He asked me why dialysis patients had to stop working and he was surprised to hear me say that he could continue working, and that his doctor and dialysis facility should be helping him work through this issue and get back to work. This story is only too common. 


