Study: An Intensive Approach to Patient Education can Help Lower Peritoneal Dialysis Patient Dropout and Decrease Peritonitis Rate
[Note: The following content reviews a study conducted by joint venture partners at the San Antonio Kidney Disease Center that was presented at the Texas Kidney Foundation in April 2017.]
End stage renal disease (ESRD) care in the United States has room for improvement in terms of associated costs and mortality. Currently, ESRD patients comprise about one percent of the Medicare population but consume more than seven percent of the Medicare budget. Also, about 80 percent of patients started on chronic dialysis are now started with a central venous catheter (CVC), which is associated with higher costs and 80 percent higher one- to two-year mortality when compared to chronic dialysis with an arteriovenous (AV) graft, fistula or peritoneal dialysis (PD). Initiating ESRD patients on chronic PD, often in an urgent-start PD program, has been put forth as a partial solution to the CVC epidemic and high costs of ESRD care, as PD often costs about $20,000 less per year per patient than hemodialysis.
Maintaining patients on chronic PD has many unique and diverse challenges. Patient dropout from PD is a common problem with multiple causes, including death, catheter dysfunction, late surgical complications of catheter placement (such as hernia and hydrothorax), elective modality change, peritonitis (PTN), exit site infection (ESI) and peritoneal membrane failure.
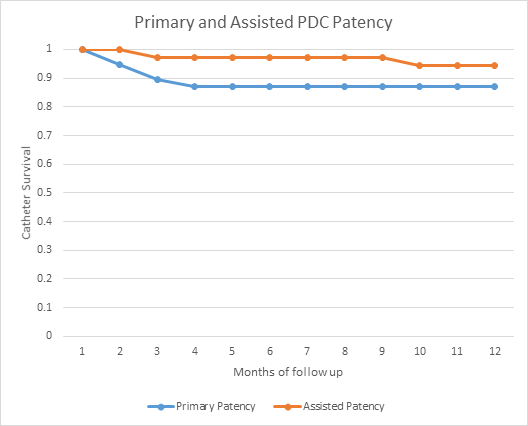
Patient education can dramatically affect patient dropout. To explore the extent of its positive effects, we conducted a study in which we instituted a new, more-aggressive patient education program focused on addressing patient dropout and PTN rates in a DaVita free-standing outpatient PD unit. Catheters were placed by fluoroscopic percutaneous technique at a local Lifeline Vascular Access center with very good catheter survival. The one-year PD catheter survival was about 94 percent, which exceeds the International Society for Peritoneal Dialysis (ISPD) recommendations of at least 80 percent one-year catheter survival.
Figure 1. PD catheters placed with fluoroscopic percutaneous technique with 94 percent one-year catheter patency.[1]
Initial dropout metrics at the PD unit
Prior to our new program, the PD unit had experienced an increase in new starts through an urgent-start PD program (in which patients started earlier than two weeks post-placement and sometimes required low-volume supine exchanges if uremic). Also, patients crashing onto dialysis via a CVC were rapidly transitioned to PD to eliminate the CVC.
About 50 percent of the new starts had limited pre-ESRD or chronic kidney disease education or preparation, which was associated with an increase in patient dropout from PD. Excluding deaths and renal transplants, the one-year patient dropout rate was 47 percent.*
Data on acceptable dropout rates are not readily available. Studies from various programs reveal a wide range of dropout rates, though typically between 20 to 30 percent per year, excluding death and transplant.
We identified the primary causes of PD dropout for our patients, and compared our data to a cohort of 128 geographically, ethnically and clinically comparable urban PD patients followed from 2009 to 2014 in Houston (the results of which were published by the Baylor College of Medicine). Comparisons included the following:
- Our incidence of dropout from catheter failure and surgical complications was very low, at 3 percent versus Houston’s 18 percent.
- Our dropout rate from PTN and ESI was lower, but still significant, at 19 percent versus 30 percent.
- Of significance was a 42 percent dropout rate in our patients due to patient preference, loss of patient ability and/or loss of social support versus only 16 percent in the Houston cohort. This led us to speculate an improved education program might be of benefit.
Figure 2. PD dropout by cause in our patient population in 2016.[1]

Improvements to the PD education program
Several changes were made to initial patient education and retraining in the unit’s standard education system. The primary modifications included:
- Spending more time with each patient, paying attention to psychosocial and family support needs. Average training time increased from six days to almost eight.
- Emphasizing earlier retraining of patients deemed to be at risk—especially during the first 90 days. Weekly physician-led, multidisciplinary meetings were held to identify patients who were at above-average risk for PD dropout, PTN or ESI. Patients starting urgently on PD were considered highest risk.
- Increasing surveillance (via home visits) of existing patients to proactively identify breaks from proper technique and to help stop bad habits from forming.
- Requiring all patients to demonstrate masking, proper handwashing technique and proper exit-site care monthly.
- Greater focus on training family members alongside the patient.
- Performing more-frequent (at least monthly) exit-site assessments and training patients to make and apply sterile hypertonic saline soaks twice daily to exit sites with evidence of trauma or irritation.
- Changing the nurse-to-patient staffing ratio from 1:20 to 1:15, with support from administration. (Urgent-start patients often need more nursing effort—to organize a social support system for any work or social issues that may complicate PD success—and are often presented to the PD unit unscheduled.)
- Placing patient education posters on exam and waiting room walls that covered relevant infection control topics, such as bleaching shower heads and the importance of identifying and preventing ESIs.
PD education program results
Without any changes in patient selection, we found that with enhanced education PTN rates decreased from one episode per 42 months to one episode in 74 months. The patient dropout rate decreased from 47 percent to 7.4 percent.**
Figure 3. Improvement in PTN rate and patient dropout rate before and after change in education program.

Discussion and Conclusion
Since starting fluoroscopic percutaneous PD catheter placement, the initiation of urgent-start patients has increased. These patients typically have less pre-ESRD education and preparation and often more psychosocial needs, which makes them susceptible to PD dropout and PTN. In our PD unit, a very low incidence of catheter dysfunction combined with a high percentage of dropout because of patient compliance, loss of social support and PTN made more-aggressive education and additional PD nursing and administrative resources very impactful on PTN and PD dropout rates. It is important to note that these results were achieved without being more selective with patients offered PD.
In our experience, the number of patients started on PD at a particular PD unit, per unit time, remains relatively similar assuming referral patterns remain generally the same. At the same time, we find that PD patient dropout tends to be a percentage of the overall census. As PD unit census increases, therefore, eventually the number of patients dropping out tends to equal the number of patients starting on PD, such that the PD unit census starts to plateau at a higher, steady number. Given typical reported dropout rates on PD of around 20 percent, addressing dropout remains a priority.
The main takeaways from our data include:
- Improved and more-aggressive patient education can have a dramatic effect on dropout and PTN rates and, in turn, patient census and patient outcomes.
- Units need to measure their dropout rates and, just as importantly, the reasons for dropout so efforts can be targeted at the biggest concern.
- Instead of setting a fixed number of days for training per patient, realize each patient is different. Increasing training beyond the minimum it takes to get the patient home can stave off problems later.
- Measuring PTN and ESI rates at 6 and 12 months is preferable to 3 months.
Although our data is somewhat preliminary we believe our experience can be generalized to other PD units that have a significant number of patients with little pre-ESRD preparation and significant dropout from patient factors and infection.
*Measured as number of dropout patients that year divided by the mean census during that year.
**Measured as number of dropout patients divided by the mean census during the reporting period. Reporting period for standard education was 12 months. Reporting period for enhanced education was four to five months.
[1] Data from the San Antonio Kidney Disease Center

Recent Comments