Kidney Patient-Centered Quality of Care, Part IV: Future Approaches to Delivering Care
Every day, as the leaders in care delivery for this vulnerable population, we should get up and think about what more we can do to ensure that our kidney patients reach the top of the quality pyramid. Increasing the investment in research to help prevent kidney disease is an aspirational, long-term goal. In the shorter term, we need to focus on the following two approaches: focusing upstream to arrest the progression of chronic kidney disease (CKD) and integrating the full continuum of care for those with end stage renal disease (ESRD).
1. Focusing Upstream
It is clear to all nephrologists that to truly optimize outcomes for ESRD patients, and to climb the quality pyramid, we must focus on patients with CKD before they need dialysis. Recent data show that nearly 80 percent of incident dialysis patients start dialysis with a central venous catheter, too few begin on home dialysis, and many have not seen a nephrologist and begin dialysis as a patient in the hospital with a higher risk for mortality.
These troubling results may be improved through CKD education programs. One such program is Kidney Smart, an ESRD-focused educational resource offered at no cost to those with CKD. The basic class is 90 minutes, during which trained educators provide interactive content on the basics of kidney disease; diet, medication and healthy habits; the importance of working with a care team; treatment options (including transplantation); and conservative therapy. In addition, one-on-one employment and insurance counseling is available so that participants understand that they can remain employed as they transition to ESRD and the many advantages of doing so. Early results of the Kidney Smart® program show that, when compared to non-Kidney Smart educated attendees, participants were:
- 2x more likely to start dialysis with a peritoneal dialysis catheter or a permanent hemodialysis access
- 6x more likely to start with a home modality
- 5 times more likely to be employed at the start of dialysis
2. Integrating Kidney Care
Focusing upstream and driving clinical programs to move up the outcomes pyramid is challenging in the fee-for-service world in which we generally operate. The true opportunity to achieve holistic, patient-centered care is through integrated kidney care (IKC)—coordination of care across the continuum of CKD and ESRD, and across care settings, which are myriad for this complex patient population.
Important components that are critical to the clinical success of IKC include:
- Nephrologists. Nephrologists lead the integrated care teams and oversee quality improvements, processes and practice retooling to support best outcomes.
- Nurse practitioners. Nurse practitioners provide renal-related care and can help manage higher-risk patients and patients who are frequently admitted to the hospital.
- Nurse care managers. Highly experienced and skilled registered nurses work closely with the patients, facility teammates, medical directors and attending nephrologists to ensure patient-centric care.
- Multidisciplinary care teams. The multidisciplinary care teams, including pharmacists, social workers, dietitians and behavioral health specialists, assist and partner with dialysis facility care teams on aspects of care that extend beyond each facility.
- Care management capabilities. Onsite and telephonic access to patients—ideally in dialysis centers—and ESRD-specific care pathways and standardized protocols can optimize the care team’s ability to deliver the highest-quality care.
- Risk stratification. Comprehensive risk stratification is performed to clearly identify areas of focus and patients most likely to transition to dialysis or be hospitalized.
The overarching goal of IKC is to keep patients healthy and avoid unnecessary hospitalizations, and thus move up the quality pyramid to enable a high quality of life. The effort is systematic and addresses the reasons unnecessary hospitalizations occur, including:
- Patients did not get the right preventive care (e.g., vaccinations, foot checks and addressing socioeconomic barriers)
- Patients did not receive adequate education or support to make healthy lifestyle choices, such as following a kidney-friendly diet
- Key adjustments to dialysis treatments were not made in a timely manner (e.g., reassessment of dry weight or medications after hospitalizations)
- Patients were non-adherent (e.g., medications were not taken or dialysis sessions were missed—sometimes due to a lack of transportation resources)
- Care was not delivered in the right setting (e.g., patients went to the ER when a phone assessment could have resolved the situation)
Case Studies: Benefits of IKC
This case study is illustrative of the deficiencies in our current fee-for-service approach and the benefits of IKC. A 49-year-old man with ESRD secondary to hypertension was on thrice-weekly dialysis but had difficulty controlling blood pressure (BP). His physician made frequent adjustments to his BP medications, but without successful control. The patient had severe headaches and paid weekly visits to the ER. When enrolled in the IKC plan, the care manager did a thorough risk assessment to determine why the patient’s BP was so difficult to control. During a visit to the patient’s home it was found that the patient had been non-adherent with his BP medications because he was supporting his wife and six children and used what little money he had to buy food and clothing for his family. Community resources were mobilized to help the family, and the patient was able to get his medications, which resulted in excellent BP control.
While this case illustrates a common problem encountered by our patients and the inadequacies of our uncoordinated care delivery system, it also shows how IKC can provide value and help us achieve the Triple Aim. The following graphic lists results achieved by DaVita VillageHealth through their IKC model.
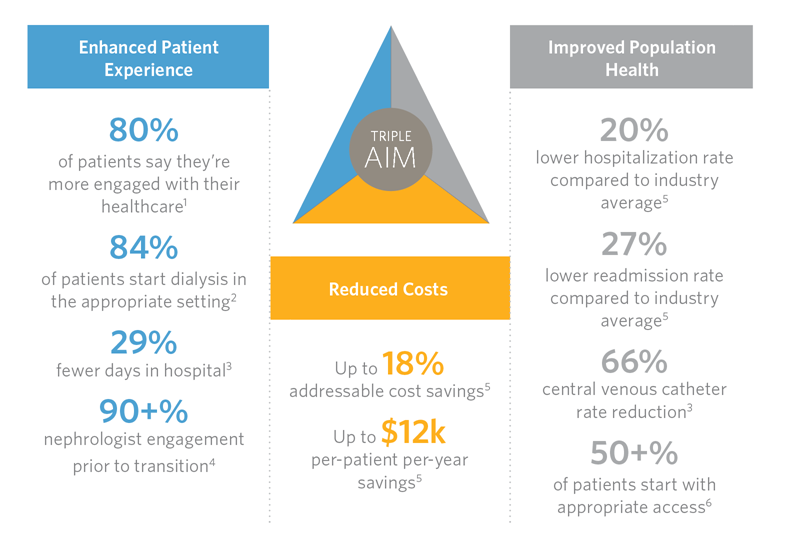
Key areas of focus for a comprehensive IKC program include fluid management, medication management, central venous catheter (CVC) avoidance and removal, transitions of care, comorbidity management, preventative care, behavioral health support and nutrition. Does intense IKC in these domains succeed on a population basis? The CVC rate in the IKC population can be reduced by 66 percent and hospitalization rates are 20 percent lower versus a comparable fee-for-service population. You be the judge.
For more information on IKC capabilities and results that can be achieved through the IKC model, visit VillageHealth.
Series Conclusion
In this kidney patient-centered quality of care series, we reviewed the current healthcare quality environment, a framework we can use to achieve quality for our patients, key participants within this framework, and approaches that can best support delivering this care. Again, our endeavors to achieve quality must be patient centric in order to be successful. We must focus on giving grandparents more moments to spend with grandchildren, musicians more moments to play their instruments and parents more moments to see their children grow. If we can give more quality moments to our patients, then we have accomplished our ultimate goal in care delivery.
Some of the content of this post has been previously published. Source: Delivering Better Quality of Care: Relentless Focus and Starting with the End in Mind at DaVita. Allen R. Nissenson, MD. Seminars in Dialysis, Volume 29, Issue 2. © 2016. Publisher: Wiley-Blackwell. [Link to original article].
1.VillageHealth Patient Satisfaction Survey, 2015. 2. VillageHealth client analysis of patients managed nine month before transitioning to ESRD. 3. VillageHealth client monthly scorecard, 2013–2015. 4. VillageHealth CKD managed members with GFR<25, 2014–2015. 5. VillageHealth client reporting, 2013–2015. 6. VillageHealth client patients Q1 2016, average from 2013–2015.

Recent Comments