February 17, 2014
DaVita Honored to Treat Patients in Saudi Arabia
The recently announced partnership of DaVita and the Kingdom of Saudi Arabia is a great opportunity to work together with an outstanding healthcare-delivery system to improve the health of its citizens. Kidney disease is an emerging public health concern in Saudi Arabia, as it is in the United States. DaVita is honored to be able to bring our knowledge and experience to enhance what is already excellent care, as well as to continue learning how best to improve care for kidney patients. This is truly a winning situation for DaVita, for Saudi Arabia and for kidney patients.
Read on below for more details on this partnership.

Left to right: Vice Minister of Health and Health Affairs, Dr. Mansour Naser Al-Howasi, Charge d’Affaires, U.S. Embassy in Riyadh, Tim Lenderking, Minister of Health, Dr. Abdullah bin Abdul Aziz Al Rabeeah, Chief Operating Officer of DaVita HealthCare Partners, Dennis Kogod.

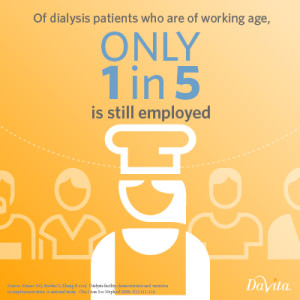 Working patients. This was a hot topic closing out 2013 and will continue to gain attention throughout 2014. Admittedly, for some patients there are medical reasons that prevent them from  working when on dialysis; however, I foresee the kidney care community turning its focus toward the education of patients, employers and the public about the benefits of continuing to work despite being on dialysis. A key part of this educational effort will be an emphasis on treatment options for patients who can continue working. For such patients, the use of home dialysis modalities is particularly helpful.
Working patients. This was a hot topic closing out 2013 and will continue to gain attention throughout 2014. Admittedly, for some patients there are medical reasons that prevent them from  working when on dialysis; however, I foresee the kidney care community turning its focus toward the education of patients, employers and the public about the benefits of continuing to work despite being on dialysis. A key part of this educational effort will be an emphasis on treatment options for patients who can continue working. For such patients, the use of home dialysis modalities is particularly helpful. 


